Introduction
In today’s rapidly evolving healthcare landscape, the integration of telehealth technologies with Electronic Health Records (EHR) is driving a transformative impact on how care is delivered and managed. Strategic telehealth-EHR integration not only enhances patient access and satisfaction but also streamlines operations, ensures regulatory compliance, and optimizes clinical outcomes. For healthcare providers and organizations seeking to remain competitive, improving care quality and operational efficiency through this integration has become essential.
This comprehensive blog explores the significant benefits of integrating telehealth with EHR systems, real-world use cases, the integration process, cost considerations, and how innovative solutions from tech leaders like TechOTD are accelerating this healthcare transformation.
Explore more about AI-driven healthcare innovations at TechOTD AI Services and browse through optimized technologies on the TechOTD blog.
Understanding Telehealth – EHR Integration
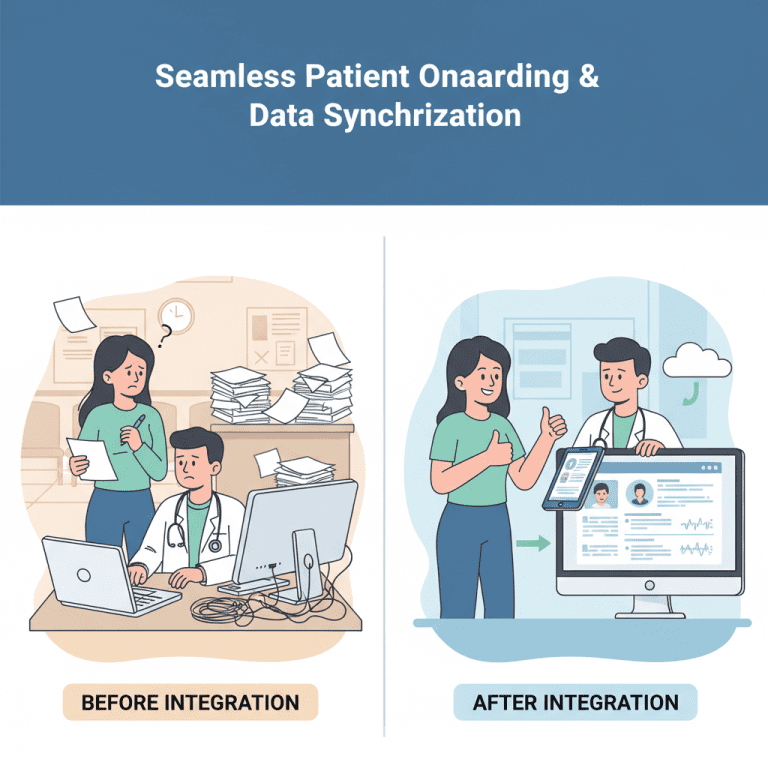
Telehealth-EHR integration enables seamless exchange of patient data between remote care platforms and centralized electronic health records. This unification supports efficient patient management, coordinated care, and real-time access to medical histories during virtual consultations. Integrated systems reduce manual data entry errors and optimize billing and documentation processes.
Key features include:
-
Real-time data synchronization for remote and in-person care interactions.
-
Unified platform for patient scheduling, documentation, and follow-up.
-
Streamlined workflows aligned with compliance requirements such as HIPAA.
For detailed AI-driven health solutions empowering such integrations, see:
Seamless Customer Journeys with AI.
Use Cases: How Telehealth-EHR Integration Transforms Healthcare Business
1. Enhanced Remote Patient Monitoring (RPM)
Integrated platforms facilitate continuous monitoring of chronic patients by syncing telehealth visits and IoT device data into EHRs. Clinicians gain comprehensive insights, enabling timely intervention and reducing hospital readmissions.
2. Virtual Consultations with Complete Medical History
Physicians access patient history instantly during video consultations, improving diagnosis accuracy and personalizing care plans without delays or fragmented data.
3. Automated Clinical Workflows
Integration automates documentation, e-prescriptions, and lab orders, reducing administrative burden and minimizing errors. This leads to faster patient throughput and billing cycles.
4. Improved Patient Engagement and Satisfaction
Patients receive consistent communication, appointment reminders, and educational resources through integrated telehealth-EHR apps, fostering adherence and trust.
5. Data-Driven Population Health Management
Aggregated data from remote visits enhances analytics, enabling preventive care strategies and outcome-based reimbursements.
The Integration Process: Step-by-Step
Implementing telehealth-EHR integration involves several structured phases:
1. Needs Assessment & Strategy Planning
Analyze existing workflows, telehealth capabilities, and EHR architecture to define integration goals. Collaborate with clinical, IT, and compliance teams.
2. Technology Selection & Architecture Design
Choose interoperable platforms and APIs, ensuring standards adherence (HL7, FHIR). Design secure data flows with encrypted channels.
3. Development & Customization
Develop connectors or middlewares, customize UI/UX for providers and patients, and incorporate AI-driven tools for analytics and automation.
Visit TechOTD’s how we work to learn about their tailored development approach.
4. Testing & Validation
Conduct rigorous integration testing, data security audits, and user acceptance testing to ensure seamless data accuracy and system reliability.
5. Deployment & Training
Roll out integrated systems gradually with stakeholder training to maximize adoption and minimize disruptions.
6. Ongoing Support & Optimization
Maintain and update the system continuously, leveraging predictive analytics to proactively address system or clinical inefficiencies.
Explore predictive analytics benefits here:
Predictive Analytics Software Development: Features, Benefits & Use Cases.
Estimated Costs of Telehealth – EHR Integration
Costs vary depending on scale, existing systems, and customization needs:
| Cost Aspect | Estimated Range (USD) |
|---|---|
| Strategy & Consulting | $10,000–$30,000 |
| Software Development | $50,000–$150,000 (API creation, middleware, UI/UX) |
| Security & Compliance | $10,000–$40,000 (Data encryption, audit frameworks) |
| Testing & Deployment | $15,000–$40,000 |
| Training & Change Management | $10,000–$25,000 |
| Maintenance & Updates | 15–25% of initial development cost annually |
Optimizing costs through AI and agile methodologies can reduce timelines and resource consumption. TechOTD specializes in delivering cost-efficient, scalable digital health solutions:
Explore Mobile Apps & AI Services.
Transforming Outcomes with AI and Emerging Technologies
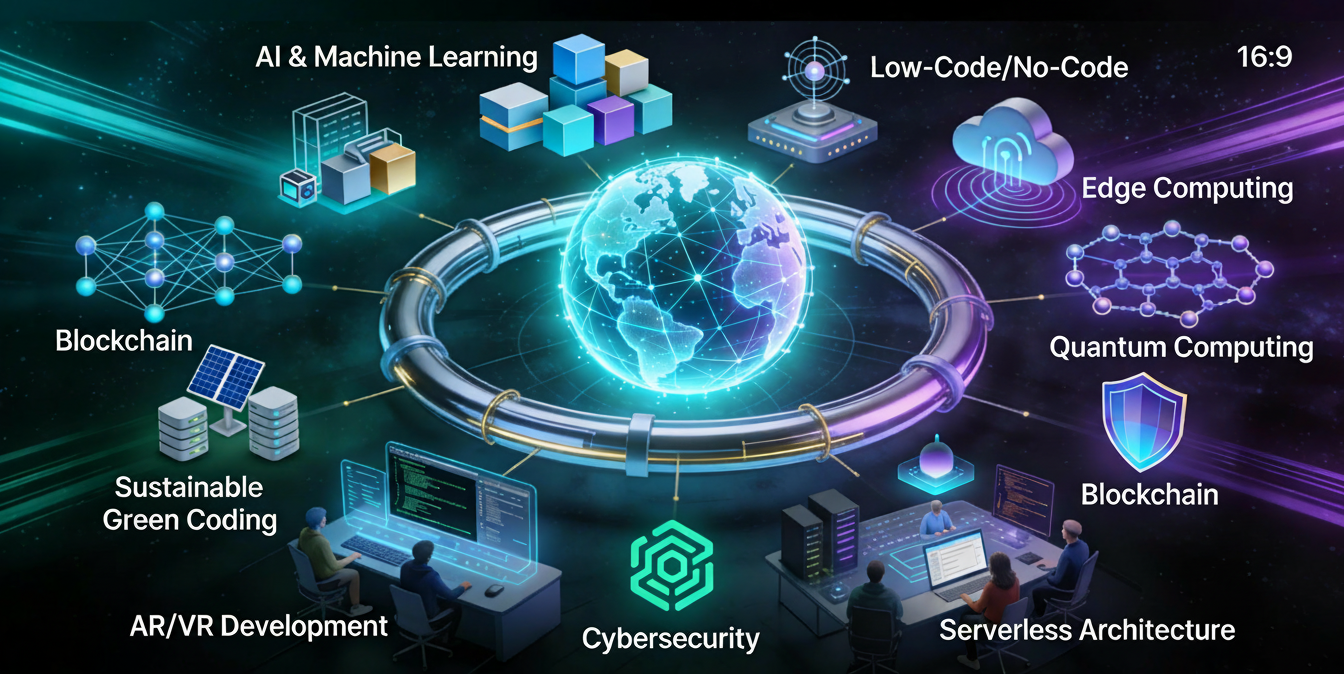
Integrating AI with telehealth and EHR unlocks powerful capabilities:
-
Natural Language Processing (NLP) for automated clinical notes and coding.
-
Sentiment Analysis to gauge patient feedback and improve service quality.
-
Predictive Models for patient risk assessment and readmission forecasting.
-
Computer Vision for remote diagnostics and image analysis.
Read more about AI trends shaping healthcare innovation:
AI Trends & Solutions – TechOTD.
Real-World Impact and Industry Insights
Leading healthcare organizations using telehealth-EHR integration report:
-
30–50% reduction in hospital readmissions.
-
Up to 40% improvement in clinical workflow efficiency.
-
Enhanced patient satisfaction scores and engagement.
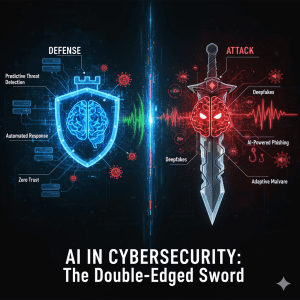
Additionally, blockchain technology integration enhances data security and patient privacy, as exemplified in Dubai’s business sector transformations:
How Blockchain Integration Is Optimizing Business Processes in Dubai.
Future Directions: Telehealth, EHR, and Beyond
The healthcare sector is rapidly evolving with IoT, AI, and cloud-powered telehealth transforming patient care. Key future trends include:
-
Interoperability advancements using standardized APIs for even smoother integrations.
-
Personalized medicine driven by AI insights from comprehensive data ecosystems.
-
Augmented reality (AR)/Virtual reality (VR) supported telehealth services.
-
Influence of emerging large language models for healthcare insight generation:
Large Language Models in Finance and Healthcare.
Conclusion
Strategic telehealth-EHR integration is a game-changer for healthcare businesses aiming to improve care quality, patient experience, and operational efficiency. By leveraging modern software practices, AI enhancements, and secure data management, organizations can not only meet regulatory demands but also gain a competitive edge. Consulting with expert technology partners like TechOTD ensures a smooth, scalable, and cost-effective integration that fuels innovation and growth.
Start your transformation journey today:
Book a Free Consultation with TechOTD and explore a wealth of knowledge in their Tech Blog.
FAQ
Q1: What are the primary benefits of telehealth-EHR integration?
Better data access, efficient workflows, regulatory compliance, and improved patient care coordination.
Q2: How complex is the integration process?
It involves multiple phases—planning, development, testing, and training—usually spanning several months depending on the system scale.
Q3: Can AI improve telehealth and EHR system efficiency?
Yes, AI automates documentation, predicts patient risk, and enhances decision-making.
Q4: What are typical costs involved in telehealth-EHR integration?
Costs range depending on scale but typically are between $100,000 to $300,000 for comprehensive setups.
Q5: How does blockchain relate to telehealth and EHR?
Blockchain enhances data security, interoperability, and trustworthiness between providers and patients.